
When the statute of limitations robs you of justice
One night in 2016, Richard Goldblatt had an acute pancreatitis attack.
“I was sitting at home, and all of a sudden I had this God-awful pain that wouldn’t go away,” he told us. The pain was so bad that at the time, I thought someone had stabbed me!”
His wife and oldest son brought him to the nearest emergency room, where medical professionals examined him, gave him something for the pain and asked him for his medical history. Richard told them he had recently removed a melanoma spot on his left shoulder, had a complete right knee replacement in 2002, and rectal repair in 2006, which had caused permanent nerve damage around the scar and, curiously, in both feet. He’d been in terrible pain ever since.
Opioids and opiates are terms used interchangeably by the media, but they mean very different things:
An "opioid" is a synthetic drug that operates directly on the brain's opioid receptors, which results in analgesia (or the numbing of pain). An "opiate" refers to that which is derived from the opium plant or synthetically created from any drug found in poppies. An opiate, therefore, is a subset of opioids.
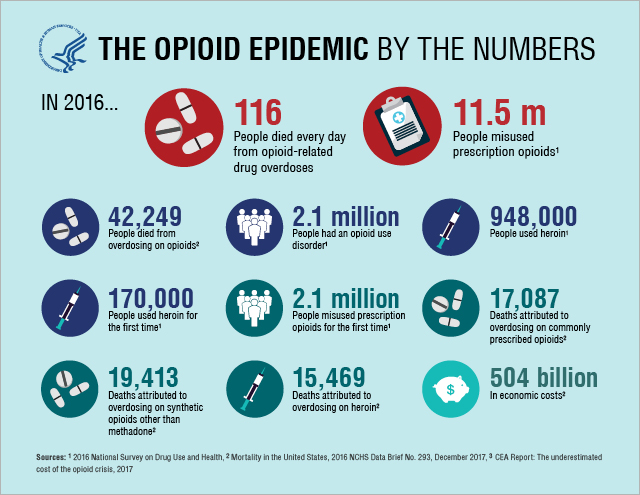
The "opioid epidemic" (or "opiate epidemic," since they are substituted for one another all the time) is the current state of political affairs regarding this type of medication. Many people are abusing heroin, oxycodone, Fentanyl and other drugs, which led to it becoming the leading cause of injury death in the United States. This necessitated the use of buprenorphine (used to treat addiction by doctors) and other medications, like Narcan (naloxone, an emergency nasal spray used to treat overdoses).
Legitimate prescriptions for opioid treatment have become much harder to come by as a result. This means that many chronic pain patients, as well as those who are post-surgical or post-injury, are left in the lurch and sometimes turn to the black market for help. The White House appointed Kellyanne Conway as its "opioid czar," which did not necessarily comfort the public because she lacks experience in this area.
This is partly why Richard is having so much difficulty getting the treatment he needs. At first, he did receive opioid medication capable of quelling his nerve pain – though that didn't last.
How the Fentanyl use began
Richard kept asking his surgeon why his feet hurt if he’d had rectal repair, as it made no sense. “He [the doctor] kept telling me it was hemorrhoid pain, and he didn’t know why my feet were hurting all the time. I didn’t find out what really happened until around 2009 or 2010, when I was finally seen by a neurologist and examined properly. He told me that the surgeon knew he’d made an error. That being said, I have suffered ever since. I was also told it was too late to have any recourse in regard to that doctor.”
Richard started seeing a pain specialist, who tried all sorts of treatments – nothing helped. They even introduced him to the most radical of treatments: the Fentanyl patch.
The Fentanyl transdermal patch is meant for people who have tried other opioid or narcotic medications and need something much, much stronger. This provides around-the-clock pain relief for 72 hours in the form of a skin patch that allows medication to sink directly into the bloodstream and absorb quickly. The list of warnings for the patch is long and thorough. Don’t take other medications with the patch. Don’t drink alcohol while using the patch. Don’t use the patch except exactly as directed by your doctor.
Richard did all of those things… and he still had problems.
“Yes, it eventually helped,” he said. “Yes, it did calm and deaden the pain... [but] I was never told about the basic warnings... I found out the hard way.”
What is Fentanyl and how is it abused?
Fentanyl is a synthetic opioid that is 50 times stronger than heroin and 100 times stronger than morphine.
It is used for severe pain that has not been alleviated by other treatments. It was first synthesized in 1960 by Janssen Pharmaceuticals, and it did exactly what it promised: It left users relaxed, pain-free and euphoric. These days, since legitimate Fentanyl pills can usually only be found in hospital settings, many have turned to the black market for illegal Fentanyl coming in from China, which seems to have set up headquarters in the state of Ohio. It's much cheaper to get a Fentanyl high than a heroin high, and the product goes much farther. Sometimes it's even mixed with other products and people don't know they're consuming Fentanyl. Economically, it makes business sense.
However, even two milligrams, used improperly, can be fatal.
Richard did not abuse Fentanyl. But, as it turned out, heat – body heat, in the case of Richard – affects the use of the patch and causes it to absorb more quickly into the bloodstream. Fentanyl patch doses are meant to last for 72 hours. Richard’s high body temperature ensured that the patch would only last one or two days.
Richard ended up in the emergency room three different times in 2017 because of withdrawal, as his body heat caused the patch to absorb medication more quickly into his body, leaving him without more Fentanyl to sustain him over the lifetime of the patch. Neither his pain management specialist nor the emergency room doctors, however, realized this at the time.
Meanwhile, after the acute pancreatitis episode, Richard began to rapidly lose weight, which made little sense because he was still hungry and eating food. Doctors put him through the paces, making him take blood tests, MRIs, CT scans, ultrasounds – all of which came back clear.
“I was led to believe that everything was back to normal,” Richard said. “I was discharged with that idea and instructed that I could go back to my life as if nothing had happened. I was back at the ER in a week.”
His frustrations were mounting. This time he was told it was gastroenteritis and that he had a list of allergies.
Richard already knew he was allergic to wheat and shellfish, so this was no surprise. He just wanted to know why he felt so awful and why he kept losing weight.
He was having new symptoms, too – he noticed an oily yellow discharge that smelled absolutely foul. When he informed his doctors, they prescribed Creon, a medication intended for exocrine pancreatic insufficiency, or EPI. This means your body is missing important enzymes it needs to digest food, and nutrients are passing through the body unabsorbed, which would explain why he was losing so much weight even though he was eating food. However, at the time, he was on such a low dose of Creon that it didn’t seem to be working.
Richard met with another gastroenterologist who wanted to do an endoscopic ultrasound, but his insurance wouldn’t cover it. Then another doctor wanted to cut out his gallbladder. Another wanted to put him on Cymbalta – “I told him, ‘No thanks.’ No more drugs in my system.”
By that time, Richard had lost almost 60 pounds. The case manager in charge of his file finally managed to get him to a doctor who could think outside of the box and diagnosed him with exocrine pancreatic insufficiency, which is what the Creon medication should have helped.
There was still a missing piece to the puzzle, however. The cause of his troubles? Opiate use.
According to his doctors, the Fentanyl he was prescribed for his progressive nerve pain aggravated an underlying pancreatic condition. As EPI is normally caused by genetics, behavior or malnutrition, it only made sense that Richard’s opiate use, which at that time was in such high dosages, threw his body into high gear and revolted against him.
Fentanyl withdrawal should be done under the supervision of a medical professional. It is an extremely addictive medication because of its euphoric tendencies, which can make users compulsive and need more to get the same effect. However, withdrawing from it properly can minimize symptoms.
Patients might supplement their withdrawal program with methadone or buprenorphine, which can lessen the severity of symptoms. A doctor might simply taper the Fentanyl, however, which is weaning the patient off until they are no longer taking it. Many users require an in-patient program to succeed.
Symptoms of Fentanyl withdrawal can include nausea, vomiting, increased pain, chills, irritability, stomach cramps and more.
Weaning off Fentanyl, the most addictive medication available
When Richard asked his doctor’s thoughts about weaning him off Fentanyl use, the doctor told him in an email that “opiates cause or aggravate a severe form of irritable bowel and will aggravate any pancreas condition you have.”
Now Richard is trapped in a physical hell against a national medical backdrop that could not be more against him.
The Fentanyl patch regimen he has been prescribed is aggravating his congenital pancreatic condition, and he cannot treat one without denying the other. If he chooses a lesser opioid, his progressive nerve pain will spike and leave him unable to physically function. If he uses Fentanyl, it inflames his damaged pancreas. Meanwhile, the statute of limitations has run out against his surgeon, depriving him of judicial remedies – as lawyers have already informed him. “I’ve been turned down a couple times,” he said.
It is a difficult climate right now in the medical field, with the opioid crisis raging across the country and even legitimate Fentanyl patch doses that are clearly not abuse being regarded with suspicion. The Drug Enforcement Agency raided the office of a prominent pain management physician, Dr. Forest Tennant, the day after he testified as an expert in a negligent homicide case. Other physicians are tapering their patients or having them sign “pain contracts,” even though they are clearly suffering on their regimens.
Then there are patients like Richard, who have medications that they need, but have suffered at the hands of doctors’ ineptitude. And who is going to pay once the statute of limitations has run out?
“I guess I’ll have to wait until I’m dead and some researcher can have my pancreas examined to prove my point,” Richard said. That is the only thing he says he can look forward to, “as this disorder will eventually kill me.”
In January 2018, Richard let us know his new pain management specialist ordered him to withdraw from the Fentanyl, as prescribing that medication was "against his principles."
On the plus side, four days into the withdrawal ("which was complete hell," Richard said), his pancreas started producing the necessary digestive enzyme again. Fentanyl had suppressed his pancreas' ability to work and made him too sensitive to medications. Now that he's gone cold turkey, he is able to eat properly – but suffers from intractable nerve pain.
"I have been told that recovering from this trip into hell could take a very long time," Richard said. The only question is whether he can handle the pain until he fully recovers.


Belinda Cartier says
Oh wow Richard!
Can you get a prescription for medical marijuana?
I take Lyrica & have a love-hate relationship with this medication but without it, my pain is unbearable!!
I’ve encountered so many awful & frightening side effects. My short term memory is obsolete anymore which has caused life to be almost unmanageable. My legs go completely numb and I’ve fallen countless times, sustaining multiple injuries. Including a spinal compression fracture that was by far the worst spinal pain I’ve ever experienced. At times my words in the middle of speaking, suddenly become so slurred and I sound intoxicated, as in drunk.! I don’t drink alcohol or partake in any illegal drugs or use marijuana. My sleep is interrupted and I sometimes can’t sleep for 2 days.
But yet, without the medication, life is unbearable due to horrendous pain in my legs.
There’s no easy answers. I do think a Doctor could remedy your situation by coming up with the best medication for your medical condition. Doctors are under great pressure to not prescribe Opioid Pain Medication and so many Chronic & Intractable Pain Patients are suffering & committing suicide because of forced tapering.
Needlessly making CPP’s & IPP’s another real victim & great tragedy in the War on Illicit Fentanyl & Heroine!
Deb Brancato says
Richard,
My heart goes out to you and your family for what you are going thru.
Chronic nerve pain caused me, as a single mom of 3, to loose my career as an RN, my house, and nearly my mind.
In 2004 a Physiatrist convinced me to go on the Fentanyl patch, which, after titration, was set at 100mcg/hr.
It worked! In time, I had my career back and bought another house. I had my life back and could be a mother to my kids.
Around 2017ish, I had begun asking my family practice doc, whom had taken over the prescription for me because I was so stable, if I could get off of the patch. We spoke about it several times and decided I should stay on it until I retired. (I will be 59 this year).
I began to hate the patch and what being on Fentynal labeled me as, even though I needed it.
I ended up with a torn rotator cuff this fall and was looking at being out of work short term disability for 5 months so I went to my doctor and insisted I be weaned off now. That was a little more than a month ago and I have gone from the 100 down to 25mcg/hr.
The withdrawal has been horrible- I’ve felt like the drug bonded with my brain, mind, emotions, even my personality. I’ve heard the drug described as a demon or a monster and I agree. Everytime the dosage is lowered I feel every withdrawal symptom in the book- but, I’m almost there and I’m so relieved.
Reading your story, I am surprised and sorry for what happened with your pancreas and the chronic pain has to be so devastating. I’m not much a person for prayer, but I will pray for you and your family.
Thanks for letting me share my story.
Deb
Melissa Gold says
Hello Deb,
Thank you for sharing your story. I’m so glad to hear that you’re so close to full recovery. Accident recovery is different for everyone, and you’re a strong person for enduring what you have and being proactive to choose the best possible recovery route to get yourself back on your feet.
Best wishes for a safe and full recovery. Take care!
Robin says
Hi Richard, I was a police officer & sustained a near death injury on duty, broken neck blown out discs in my back & shoulder injury. At first I was just taking tylenol as after 6 months I went back to work but after a year the pain was so bad I was forced to take a medical retirement. Gradually my doctor at the time put me on more & more meds topping out at 8 hydrocodone a day, 100 microgram fentanyl patch, Soma & a second muscle relaxer, ambien & monthly injections in my shoulder. Once people started dying from opoid overdoses I went back to my doctor wanting to discuss weaning off some of the meds but when I arrived for my appt I was informed she had left her practice with no warning! I had to scramble to find another dr fast & luckily I found a good one. Over the course of 2 years I was able to wean off everything except the hydrocodone of which I only take one a day now. Then out of nowhere 2 yrs ago, like you, I started having serious digestive problems & am still having tests done to figure out the problem but the tests keep comming back showing nothing wrong. My new GI doctor now thinks my problems are the result of prolonged use of prescribed opioids by my previous doctor! Like you, I would love to sue her for malpractice, as she should have known better, but I can’t even find her. I’m getting ready to contact some lawyers & a private detective to locate her & see what can be done. The doctors we see took an oath to do no harm & we had doctors who harmed us greatly & it’s we who are paying the price not the doctors who got us addicted! We also need to work with state legislators & the medical board to extend the statute of limitations in our types of cases so we can receive some justice. I feel that if doctors can’t be sued because your symptoms didn’t show up for several years, they will continue to harm others because there aren’t any consequences for what they did to us! I hope that you’re still progressing in your recovery. I am doing better now, I work with a nutritionist, health coach & a psychologist all at no cost to me. I’ve found that deep meditation, pilates & a bi-weekly session with a massage therapist has helped me alot. I truly hope you can find a path that will help!
Ian Pisarcik says
Thanks for your thoughts, Robin.
FITORU says
I enjoyed reading your story. Im looking forward to read more of your posts.
Ian Pisarcik says
Thank you for the comment!
NYC Workers Comp Dr says
Thanks for sharing
Melissa Gold says
Thanks for reading! I’m glad the piece was helpful to you.